Lung Tumour Ablation
Lung ablation is a minimally invasive, image-guided procedure used to treat primary lung cancers or metastatic lung lesions in patients who are not suitable candidates for surgery.
Overview
Lung ablation is a minimally invasive, image-guided procedure used to treat primary lung cancers or metastatic lung lesions in patients who are not suitable candidates for surgery. Performed by Interventional Radiologists (IRs), the technique uses heat (thermal ablation) or cold (cryoablation) to destroy cancerous tissue while sparing surrounding healthy lung. It can be an effective alternative to surgery or radiotherapy, particularly for patients with limited lung function, multiple comorbidities, or small, localized tumours.
What is Lung Ablation?
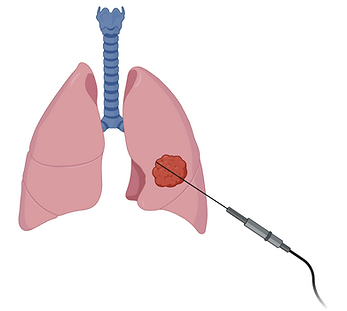
Lung ablation involves inserting a thin probe (ablation needle) through the skin and into the lung tumour under CT guidance. Once accurately positioned, the probe delivers either high-frequency electrical energy (radiofrequency ablation), microwave energy (microwave ablation), or extreme cold (cryoablation) to destroy cancer cells. The treatment causes the tumour cells to die and be gradually reabsorbed by the body.
The procedure is almost always performed under general anaesthesia, though can sometimes be performed with conscious (twilight) sedation depending on the lesion location and patient needs. Lung ablation may be used alone or alongside other treatments such as chemotherapy, immunotherapy, or radiation; in a multidisciplinary approach by interventional radiologists, oncologists, and radiation therapists.
Who is Lung Ablation suitable for?
Lung ablation is commonly used for:
-
Early-stage non-small cell lung cancer (NSCLC) in patients unable or unwilling to undergo surgery
-
Lung metastases from cancers such as colorectal, renal, breast, or sarcoma
-
Patients with limited disease burden, usually fewer than 3 lesions, each <3 cm in diameter
-
Individuals with compromised lung function or other conditions making surgery high-risk
Your oncology team and interventional radiologist will assess your imaging, tumour type, overall health, and treatment goals to determine if you are a suitable candidate.
Effectiveness
Numerous studies have demonstrated that lung ablation provides excellent local control for selected tumours, particularly when:
-
Tumours are small (typically <3 cm)
-
Located in peripheral (outer) areas of the lung
-
Treated early in the disease process
Key advantages include:
-
Local tumour control rates of up to 90% for small lesions
-
Preservation of lung tissue and pulmonary function
-
Repeatability – ablation can be safely repeated if new lesions appear
While lung ablation is not curative in all cases, it can significantly extend survival, improve quality of life, and delay progression of disease when used in appropriate circumstances.
Procedure
-
Consultation: Your case will be reviewed by a multidisciplinary team, including an interventional radiologist, to determine suitability.
-
Preparation: You may be required to fast for several hours prior. Pre-procedure imaging will inform procedural planning, and you will be provided personalised information & instructions specific to your procedure.
-
Ablation: The procedure is typically performed under sedation or general anaesthesia. A small needle is inserted into the lung lesion under CT guidance, and the ablation is performed over 10–30 minutes. Total procedure time is expected to be around 1-2 hours, depending on number and location of lesions.
-
Post-Procedure Care: You will be monitored in recovery for several hours. A chest X-ray is performed to check for complications like pneumothorax (collapsed lung). Most patients stay overnight and go home the next day.
Benefits
-
Minimally invasive, with fewer complications than surgery
-
Effective for small tumours and solitary metastases
-
Can be repeated if new lesions develop
-
Short hospital stay and quicker recovery compared with surgery
-
Preserves lung function and quality of life
Risks and Considerations
While lung ablation is generally safe, risks include:
-
Pneumothorax (air leak or lung collapse), requiring chest tube placement in some cases
-
Bleeding at the puncture site or into the lung
-
Post-procedural pain or cough
-
Infection or rare damage to nearby structures
-
Incomplete ablation, particularly with larger or central lesions
Specialist Expertise
Interventional Radiologists (IRs) are uniquely specialty trained in both the advanced imaging assessment and grading of lung tumours and image-guided "pin-hole" procedures including biopsy and ablation. Interventional Radiologists (IRs) are broadly experienced in ablation procedures as they undergo comprehensive dedicated training in Radiofrequency Ablation (RFA), Cryoablation, and Microwave Ablation (MWA) of tumours throughout the body, including the kidney, liver, lung and thyroid.
Is Lung Ablation Right for You?
You may be a candidate for lung ablation if you:
-
Have one or a few small lung tumours not suitable for surgery
-
Have medical conditions limiting your surgical options
-
Are looking for a local, tissue-preserving treatment
-
Require additional local therapy in a broader cancer treatment plan
Decisions are made in close collaboration with your oncology team, and all treatment options will be carefully explained.
Preparation and Referral
If you would like to consult with an Interventional Radiologist about renal tumour ablation, please send a referral for consultation, including the following
-
CT and other imaging results
-
Blood tests including coagulation
-
Records of consultations with other doctors and specialists
Public eligible patients can undergo the treatment with no out-of-pocket expense in the public system. Lung ablation is performed at most of our public and private hospital locations in Melbourne, Victoria, Australia.
Lung ablation content by Dr James Lisik.