Rectal Artery Embolisation
Rectal Artery Embolisation (RAE), or Haemorrhoid Embolisation, is an emerging minimally invasive procedure to treat internal haemorrhoids by reducing their blood supply.
Haemorrhoidal Disease
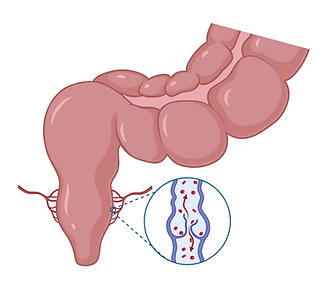
Haemorrhoids are abnormally enlarged vascular structures located in the lower rectum and anus, and haemorrhoidal disease affects up to 40% of the population. When these structures become inflamed or swollen, they can cause a range of symptoms including bleeding, pain, itching, and discomfort. Haemorrhoids are generally classified into two types:
-
External haemorrhoids, which develop under the skin around the anus
-
Internal haemorrhoids, which form inside the rectum above the dentate line
Internal Haemorrhoids
Internal haemorrhoids, the primary target for Rectal Artery Embolisation (RAE), are typically not visible externally. They often present with painless rectal bleeding, especially during or after bowel movements. In more advanced cases, internal haemorrhoids can prolapse (protrude outside the anus) and may become painful. These haemorrhoids are graded from I to IV depending on severity. RAE is typically considered for patients with Grade I to III internal haemorrhoids who have not responded well to conservative measures such as dietary changes and topical treatments.
External Haemorrhoids
External haemorrhoids, on the other hand, may cause pain, swelling, and itching, especially if a clot forms (thrombosed haemorrhoid). These are not treated with embolisation. Management typically includes topical medications, sitz baths, increased dietary fibre, and in some cases, minor surgical procedures.
What is Rectal Artery Embolisation?
Rectal Artery Embolisation (RAE), or Haemorrhoid Embolisation, involves the selective occlusion of the arteries supplying the haemorrhoidal tissue—primarily the superior rectal artery—using embolic materials such as microcoils or particles. By reducing the blood flow to the haemorrhoids, the procedure alleviates symptoms and promotes shrinkage of the haemorrhoidal tissue.
Effectiveness
Clinical studies have demonstrated the efficacy of RAE in managing haemorrhoidal symptoms:
-
Significant reduction in rectal bleeding and improved quality of life scores in study populations, with an excellent safety profile
-
Recurrence rates (~20%) that are similar or better than those for rubber band ligation (~50%) and surgical haemorrhoidal artery ligation (~30%) at 12 months (M. Nguyenhuy et al., 2022)
-
Minimally invasive nature leads to significantly shorter recovery times and reduced morbidity compared to traditional surgical methods
Procedure
-
Consultation: An interventional radiologist will assess your condition through a clinical evaluation and imaging studies to determine suitability for RAE.
-
Preparation: The procedure is typically performed under local anaesthesia with sedation; but can also be performed under general anaesthesia. A catheter is inserted through a small incision in the groin (femoral artery).
-
Embolisation: Using fluoroscopic guidance, the catheter is navigated to the superior rectal artery. Embolic agents are then delivered to block the blood flow to the haemorrhoids.
-
Post-Procedure Care: Patients are typically monitored for about four hours post-procedure and can often return home the same day. An overnight admission may be preferred in some circumstances and can be discussed with your treating IR. Mild discomfort or cramping may be experienced but typically resolves within a few days.
Benefits
-
Minimally invasive, with no surgical incisions
-
Preservation of anal sphincter function, reducing the risk of incontinence
-
Typically performed as an outpatient procedure with rapid recovery
-
Effective symptom relief for patients unresponsive to conservative treatments
Risks and Considerations
While RAE is generally safe, potential risks include:
-
Minor bleeding or bruising at the catheter insertion site (groin or wrist)
-
Transient pelvic pain or discomfort
-
Rarely, non-target embolisation leading to unintended tissue damage
It’s essential to discuss potential risks and benefits with your healthcare provider to make an informed decision.
Is RAE right for you?
RAE may be suitable if you:
-
Experience persistent haemorrhoidal symptoms (particularly bleeding) despite conservative treatments
-
Prefer a minimally invasive option over traditional surgery with similar treatment outcomes
-
Seek a treatment with a shorter recovery period
A thorough evaluation by an interventional radiologist will determine your eligibility for the procedure.
Specialist Expertise
Interventional Radiologists (IRs) are specialty trained in the care of patients undergoing rectal artery embolisation, also referred to as haemorrhoid embolisation, including the pre-procedural assessment, operation and post-procedural care. Interventional Radiologists (IRs) are extensively experienced in embolisation procedures as they regularly perform embolisation in many areas of the body, including the lung, liver, spleen, kidney, bowel and pelvis.
Multidisciplinary Care
It is important that you consider all main treatment options for haemorrhoids, which includes dietary measures, topical treatments and surgical procedures. After consultation with our interventional radiologist, your case may be discussed with or you may be referred to consult with a colorectal surgeon if you haven't previously seen one.
Preparation and Referral
If you would like to consult with an Interventional Radiologist about rectal artery embolisation, please send a referral for consultation, including the following
-
Imaging and blood test results
-
Records of consultations with other doctors and specialists
Public eligible patients can undergo the treatment with no out-of-pocket expense in the public system. Rectal Artery Embolisation procedures are performed at most of our public and private hospital locations in Melbourne, Victoria, Australia.
Rectal Artery Embolisation (RAE) content by Dr James Lisik.
